A Home Run Breakfast With Diabetes
Seven things I do to beat the hardest meal of the day.
With diabetes, the stakes are high in the morning. A well-managed breakfast can dramatically improve my time in zone (70-140 mg/dl) for the rest of the day. Conversely, I might regret poor choices at breakfast three, five, even eight hours later.
Unfortunately, the morning brings a perfect storm for blood sugar spikes: high-carb and sugary food options, insulin resistance and inactivity, time demands, stress, and caffeine.
Breakfast is also the most likely meal to prompt outrage: “How can I be LOW right now?! I did the same thing yesterday and was HIGH!”
This article shares what I’ve learned through diabetes trial-and-error about managing breakfast with diabetes, including many personal examples collected over the past few weeks. The tactics that have had the biggest impact on my diabetes are listed first, though all seven have made a major difference. Click on a tactic in the table of contents below to skip right down to it.
At the end of the article, I’ve added two other approaches that might improve blood sugar around breakfast (cut caffeine and reduce stress), but I couldn’t confirm them from my own data. Please send feedback or other tactics by email or on Twitter; I love hearing from readers! And if you find this article useful, check out my upcoming book, Bright Spots & Landmines!
I’m NOT a healthcare provider.
Always
confirm changes with a professional, especially when using insulin.
Summary
- Cut carbs. I often eat scrambled eggs or nuts for breakfast.
- Eat non-traditional foods for breakfast: almond flour, nuts and seeds, lentils, etc.
- Dose insulin 20+ minutes before eating carbs, and wait longer if blood glucose is above target or when eating something really sugary.
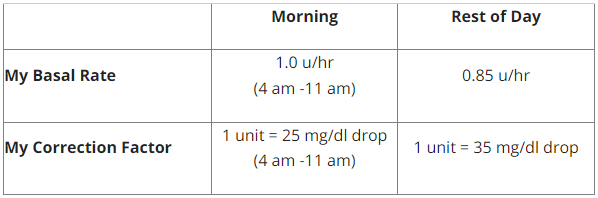
- More breakfast insulin: I use a more aggressive morning correction factor and more early morning basal to cope with higher AM insulin resistance.
- Be active, especially by walking after breakfast.
- Get real-time glucose data to course-correct after breakfast, learn what works, and optimize overnight insulin.
- Eat a smaller, earlier dinner and don’t snack around bedtime.
My Tactics for a Homerun Breakfast
1. Cut carbs. I often eat scrambled eggs or nuts for breakfast, which bring five big advantages: no need to take insulin earlier (#3 below), no burden to carb count, smaller doses of insulin, lower glucose spikes, and more predictability. Eggs are not a concern for raising cholesterol (according to the US government’s latest dietary guidelines), are a great way to sneak in vegetables via a veggie scramble, and take just four minutes to make (I timed it). Nuts require no prep at all, are portable, and available pretty much everywhere (even at gas stations and airports). I generally take one unit of insulin right when I start eating eggs or nuts, which helps cover the rise in glucose from protein and fat. If I’m low or following exercise, I may take no insulin at all.
Here are some typical egg and nut breakfasts I’ve eaten recently, tracked using Meal Memory and Dexcom G5. I’ve been buying these amazing low-carb tortillas lately (10 g of carbs, of which 7 g are fiber), which don’t raise my glucose and make it an egg breakfast wrap!

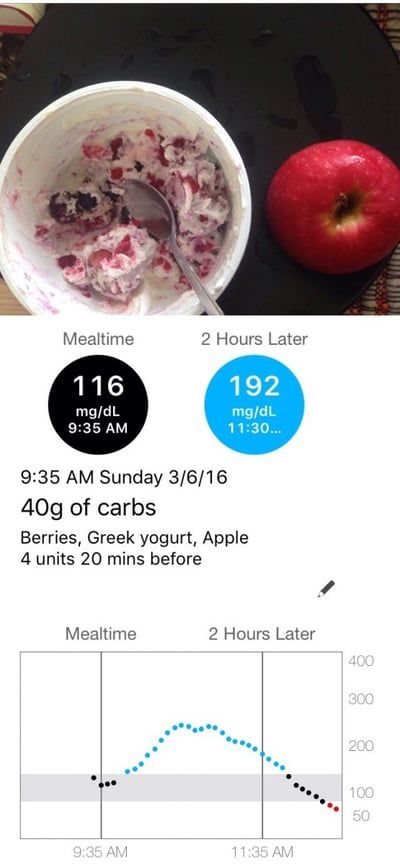
Here’s what happened when “I did everything right!” with a higher-carb, nutritious breakfast last week. I choose whole foods (berries, plain Greek yogurt, apple), measured the carbs out, took insulin 20 minutes before eating, and started at a blood sugar of 116 mg/dl. I was over 250 mg/dl within one hour! I definitely needed more than a 20-minute head start (see #3 below), but this was probably a best-case scenario – it wasn’t Honey Nut Cheerios or waffles with orange juice. I find that high-carb breakfasts make diabetes really difficult.
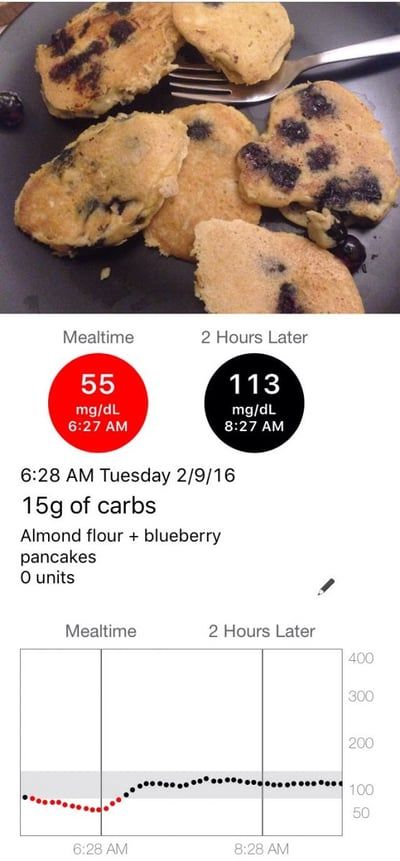
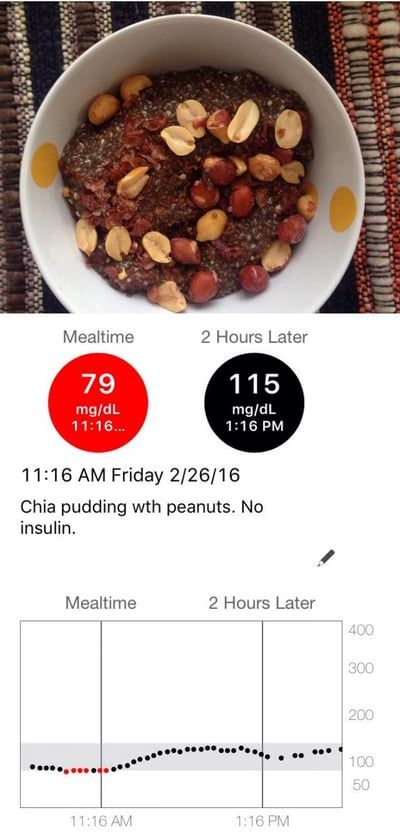
2. Eat non-traditional foods for breakfast: almond flour, nuts and seeds, lentils, dinner leftovers, etc. Almond flour has been the most unexpected win, since it has reintroduced pancakes and bagels into my life. But who says breakfast has to be traditional? Sometimes I’ll eat lentils or dinner leftovers for breakfast. In Europe last month, I ate cold cuts at hotel breakfasts. I’ve also been experimenting with Chia pudding, which doesn’t seem to change glucose at all (though I’m still looking for a tasty recipe). Here are two examples (almond flour pancakes on left, chia pudding on right):
3. Insulin head start: dose
20+ minutes before eating carbs, and wait longer if blood glucose is above target or when eating something really sugary.
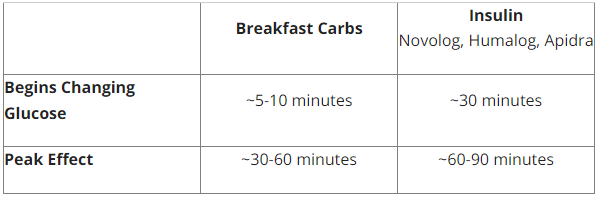
I usually opt for cutting carbs (#1), since I’m impatient, find this head start hard to remember, and often need more than 20 minutes (e.g., when starting at a morning glucose of 180 mg/dl, I might need a 40-minute insulin head start). Here’s what I’ve generally observed for myself, though these estimates vary by type of food and person:
4. More breakfast insulin: I use a more aggressive morning correction factor and more early morning basal. These strategies help counteract the insulin resistance I usually experience around breakfast, particularly when I don’t get enough sleep (see below). Many patients I know also use a more aggressive insulin-to-carb ratio in the morning (e.g., 1:8 instead of 1:10). The best way I’ve found to optimize these settings for myself is described in #6: getting real time glucose data to inform my decisions.
[Note: This is highly individual – always work with a healthcare professional before changing your insulin doses.]
5. Be active, especially walking after breakfast.
Morning exercise (I do cycling or strength training) increases my sensitivity to insulin and makes it far easier to deal with breakfast. As a bonus, AM activity also cuts my stress and clears my head to start the day. Even a short walk after eating breakfast (20 minutes) can dramatically reduce my blood sugar (-50 mg/dl or more), particularly if I have some insulin on board. Here are two recent examples of short post-breakfast walks; in the second example, I took a bit too much insulin after eating lentils.

6. Get real-time glucose data to course-correct after breakfast, learn what works, and optimize overnight insulin. Wearing CGM (Dexcom G5, Medtronic Enlite) or Flash Glucose Monitoring (Abbott FreeStyle Libre) has three main advantages for dealing with the unpredictability of breakfast:
- Course corrections – no two mornings with diabetes are the same. Real-time glucose data gives me actionable feedback to make changes on the fly: “I’m going high; maybe I need some more insulin” or “I’m going low; I need to eat something.”
- Learn what works. Before getting on CGM six years ago, I ate granola bars, cereal, and oatmeal for breakfast; I rarely eat those foods now (only before 2+ hour bike rides).
- Wake up at a better glucose. Breakfast is easier when I wake up at 100 mg/dl instead of 180 mg/dl, and wearing a sensor has helped me uncover overnight problems, wake up when I’m high or low, and adjust insulin accordingly. I now get out of bed in zone (70-140 mg/dl) more often, which gives me a head start on breakfast.
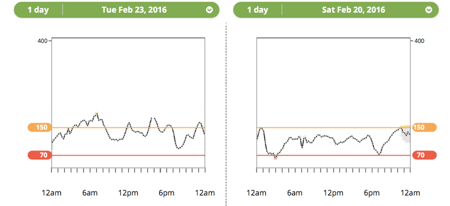
7. Eat a smaller, earlier dinner and don’t snack around bedtime. When I wake up high (over 160 mg/dl), it’s often because I ate a large dinner after 8pm the night before, or I snacked on too many nuts close to bedtime. I’m more likely to wake up in zone (70-140 mg/dl) if I have dinner early (6-7:30 pm) and don’t eat after (unless I’m correcting a low).
- The picture below compares two examples: a later dinner close to bedtime (left side) vs. nothing near bedtime (right side). The respective next days don’t always happen like this, of course, though I find a big dinner late in the day is pretty much always a bad idea. This tactic makes a big difference often enough that it’s one of my 10 diet commandments (#8).
Hypothesis I Couldn't Confirm:
1. Cut caffeine? Caffeine can raise blood sugar, meaning less morning coffee or tea (or using decaf) could prevent glucose spikes. I didn’t give this a head-to-head test to confirm, and think it’s probably a smaller factor relative to other drivers (see above). I drink a huge French press of loose leaf green tea every morning, which seems to raise my glucose anywhere from 0 mg/dl to 30 mg/dl. Tea does have less caffeine than coffee, meaning java drinkers might see a blood sugar benefit from switching.
2. Reduce morning stress? Stress can raise blood glucose, but I’ve found it challenging to pair cause and effect here – do I have lower post-breakfast blood sugars with lower stress, and higher AM blood sugars with more stress? Possibly. Exercise definitely reduces my stress, but it also reduces glucose on its own. Meditation also reduces my stress levels, though I’ve never seen an immediate glucose benefit from doing it. Striving for less stress is a good thing regardless of how it impacts blood sugar, of course! More on stress here.
https://diatribe.org/why-diabetes-and-life-so-stressful Let me know by email or on Twitter; I’ll add new tactics here!
Credited: [Author:
Adam Brown], [Source: diaTribe Learn MAKING SENSE OF DIABETES], [Site: https://diatribe.org/]
Healthy Bites