7 Common CGM Hang-Ups (and How To Get Around Them)

Key takeaways:
- Some simple planning and quick adjustments can help your CGM stay connected.
- Positioning, application and adhesion tips can assist in keeping sensors in place and avoiding skin irritation.
- Online communities are a great place to find suggestions for specific CGM issues from people with diabetes.
Continuous glucose monitors provide invaluable insights into the steady work of managing blood sugar levels; here are a few tips for day-to-day use that can make your CGM more secure, accurate, and comfortable.
Read on for hard-won advice from personal experience and professional guidance for staying ahead of potential issues before they start.
1. The hang-up: Getting your CGM caught on stuff
The scenarios for unintentionally pulling off your CGM sensor are multiple and varied. Door jams, dining tables, and toddling children are all accomplished sensor snaggers. Just taking off a t-shirt a little too enthusiastically – or putting one on – can also take the sensor with it, and the cannula doesn't have to come out fully to stop working.
Placing the sensor on the back of your arm can help, but you may find even there, when you pivot in a tight space, the sensor will sometimes get caught.
The solution
Thankfully, there are many ways to secure your sensor, easily found in online stores, and after trial and error people tend to land on a favorite. You'll find products that make skin sticky before applying the sensor. Or you can buy fabric overlays that reduce the chance of catching your CGM on something. Skin Tac is one of the more popular products for increasing adhesion. Tegaderm is a thin, clear film used by many people to secure CGMs, and it has the added benefit of reducing skin irritation, a common issue. (See more products that can help with adhesion.)
2. The hang-up: Irritated skin at your CGM site
Irritated skin is the bane of many CGM users, when the material or adhesive that holds the sensor on your body causes an unpleasant interaction.
The solution
In addition to keeping sensors secure, products that provide a barrier, including Skin-Prep and Skin Tac, can provide protection from irritation when applied before the sensor.
Other techniques like careful rotation and letting the sensor air out before applying it can also help.
Experienced CGM users often post about their experiences with specific products online, good and bad, which brings us to our next tip.
3. The hang-up: Even after consulting your doc, you still have questions
Healthcare pros can't envision every potential scenario related to CGM use, and life happens between doctor appointments.
The solution
A 2023 study found that people using social media to research CGMs saw benefits in self-management, cost, and blood sugar management. The researchers also saw an opportunity for other researchers as well as diabetes specialists and other providers to engage in these communities.
Some of these online communities have thousands of users. Facebook groups such as CGM in the Cloud are a good place to start. Reddit communities, sometimes called subreddits, can also be helpful. Try searching in a web browser for your specific issue plus "Reddit" to find threads that can address your needs. Whatever issue you're facing, others have likely been in the same boat, and clever workarounds are sometimes a click or tap away.

4. The hang-up: False lows
Compression lows, which lead to false low readings, can occur when sleeping in certain positions. When lying on the sensor, this pressure reduces the volume of interstitial fluid from which blood glucose is measured. Less volume can translate to less glucose, then incorrect low readings and alerts.
This problem is sometimes compounded by treating the false low with fast-acting carbs, leading to high blood sugar levels.
The solution
The ways to avoid compression lows are simple if somewhat restrictive. Give some thought to how you sleep when inserting your sensor so that it's not likely to be squashed by your bed, pillow or covers. You can also find arm band covers online that can help.
If you suspect a compression low, you can verify the blood sugar reading with a finger stick before treating. A series of steady readings followed by a sharp drop is one potential sign of a compression low. If this is an ongoing issue, talk to your health care provider about ways to avoid them and potentially take a few minutes to let the CGM reading correct if you suspect a compression low.
5. The hang-up: Your CGM expires at an inopportune time
CMG sessions have a way of ending at the worst moments, for example during the middle of the night or very early morning, when you're heading to work or an appointment, or when you're in public or traveling without a convenient spot to start a new sensor.
The solution
One simple way to avoid these hangups is to plan to make the sensor change at the same time of the week, first thing in the morning. That way you have plenty of time to remove and apply the new sensor, and a predictable time for when you'll need to remove it next.
Some CGM users insert a new sensor two hours before the old one expires, a process called "soaking" that allows the new sensor to acclimate to the body. This can help make the readings more accurate when the new sensor begins, avoiding the incorrect readings from a new sensor that some people see shortly after starting.
6. The hang-up: You have CGM application anxiety
Inserting the sensor is frequently painless, but the accompanying mechanical click from the applicator can be slightly alarming to some.
The solution
Grab some headphones or earbuds for you or your child and put on some favorite music or a video on your phone.
Research has shown music therapy can reduce distress and pain in children who are experiencing brief medical interventions; for teens, active distractions like a video game and passive ones like watching an online video have been shown to be helpful. You can find more strategies in this study from the Canadian Paediatric Society, including approaches for infants.
7. The hang-up: Alarms are too loud (or soft)
If you sleep soundly, first: Congratulations on your blood sugar management wizardry. But if you also sleep through your CGM alarms, you might consider ways to make the alarms more noticeable.
The solution: Find the alert that works for you
To make alarms louder you can pair your phone with a Bluetooth speaker by your bed, which can significantly increase the alert volume. Some people simply set their CGM receiver or smartphone app to vibrate then place it in a glass or plastic bowl next to their bed which will shake things up (sorry) and make a noise that will wake heavy sleepers.
To make alarms louder you can pair your phone with a Bluetooth speaker by your bed, which can significantly increase the alert volume. Some people simply set their CGM receiver or smartphone app to vibrate then place it in a glass or plastic bowl next to their bed which will shake things up (sorry) and make a noise that will wake heavy sleepers.
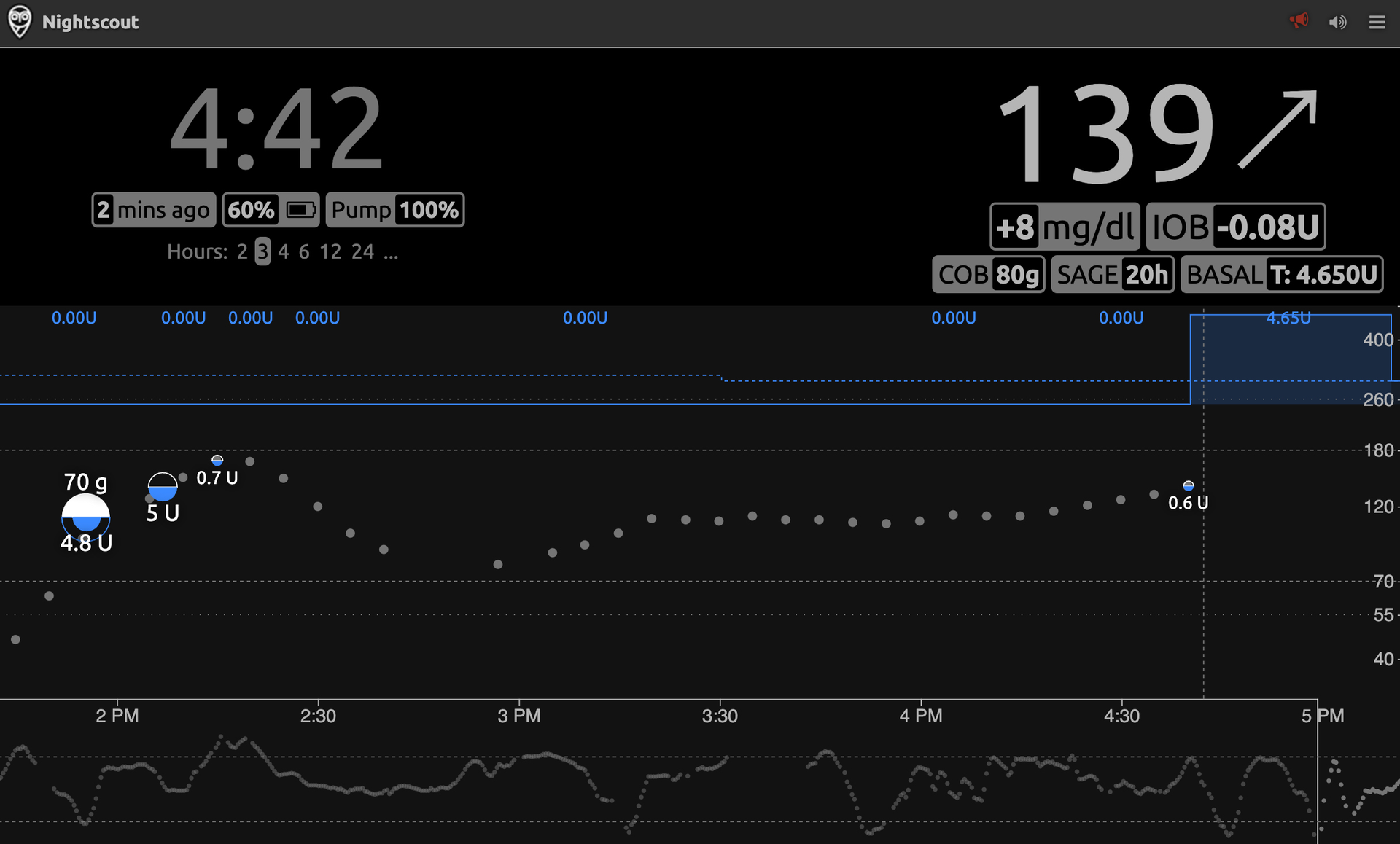
Nightscout is an open-source, DIY project that allows users to visualize their CGM and treatment data. The service can be used to create customized alerts.
If you're a bit more technically motivated you can set up Nightscout, a DIY community-created site that displays CGM and treatment data, like meals and insulin doses on a password-protected web site. Nightscout has alerts some users find useful, but it can also act as a way to connect your CGM to a range of other services. One of those services is the SugarPixel device (it looks like an alarm clock with your readings), which is widely used by people who are deaf or hard of hearing or blind or have vision loss.
The SugarPixel can be connected to a number of add-ons that alert users with flashing lights, or a vibrating device that slides under a pillow. These alerts may also be a welcome change for your significant other compared to recurring alerts when they are trying to sleep.
If your alarms wake up your partner, consider switching your CGM to the vibrate setting before bed, as well as before heading into a meeting, movie, important life events (that relatives won't let you live down for interrupting) and other places where audible alerts are undesirable.
Anyone who's worn a CGM sensor has likely run into a few of these issues leading to inaccurate readings, missed alerts or lost connections. But with a little planning, and a few small adjustments, they can frequently be avoided.
Healthy Bites















